Immune System: Nature vs. Nurture
Immune System: Nature vs. Nurture
By Carina Venter, Allergy Dietitian
The development of the infant’s immune system starts very early
on in pregnancy. This process continues into old age and is
affected by dietary and environmental factors throughout the life
cycle: gestation, infancy, toddlerhood, childhood, adulthood and
old age. Midwives, health visitors and nursery nurses are often
the first line of contact regarding any problems pregnant women
or parents of infants/young children may experience. It is
therefore important that Healthcare Professionals should
understand the development of the infant’s immune system and
be aware of factors that could be beneficial or detrimental to
this process.
These factors were discussed at a round table meeting, which took
place on Friday 26th May 2006 in Guildford. The panel consisted
of experts in the field of immunity, allergy and nutrition who
participated in authoring the three preceding feature articles on the
infant immune system*. The members are listed below:
Members
Jane Clarke, Panel Chair and Nutritionist, The Times
Dr. Amolak Bansal, Consultant Immunologist and Allergist
Carina Venter, Allergy Dietitian
Rosan Meyer, Paediatric Dietitian
Following on from these articles and the meeting, the panel felt that
this information should be shared with Healthcare Professionals and
felt that aspects involved in the developing immune system can be
described best in terms of physiological and genetic factors (nature)
and nutritional and environmental factors (nurture).
Nature
Development of the immune system during pregnancy
Two factors play an important role in-utero in the development of
the infant’s immune system: the maternal diet and the maternal
immune system(1).
– The mother’s diet provides the foetus with all the nutrients
required for the developing immune system
– The maternal immune system changes during pregnancy to
promote tolerance to the foetus. This change involves a shift
towards the “allergy prone” (Th2 cells) immune response. It is
therefore important that the balance between the “allergy
prone” cells and the cells that are required to kill infected or
damaged cells (Th1 cells) is restored at birth or shortly
thereafter(2,3)
Continued development of the immune system shortly after birth
A baby is born with an immature immune system, making the post
partum days a vulnerable time during which they can be at
increased risk of infection. Breastmilk is best for a baby as it can
help to strengthen their developing immune system. Breastmilk
can help to protect against gastrointestinal and respiratory
infections (4, 5, 6) and is associated with protection against the
development of some allergies (7, 8).
About two thirds of the infant’s immune system is located in the gut.
The infant’s gut is in close contact with bacteria and food proteins
and has to decide which ones will be absorbed and which ones
need to be kept out (9).
However, the infant’s gut may be unable to cope with this “burden”
and needs to be supported with the following:
– Prebiotics and long chain polyunsaturated fatty acids (e.g.
omega-3 fatty acids) increase colonization of the gut with
friendly bacteria and degrade large food proteins (10)
– Friendly bacteria such as bifidobacteria and lactobacillus,
enhance the immune system (11) and can help to produce a
balanced T-helper cell response i.e. a balance between Th1 and
Th2 cells. Some studies have shown that prebiotics increase the
number of friendly bacteria in the infant’s gut (12) and there is
emerging research which suggests prebiotics may even help to
reduce the risk of developing eczema (13)
The infant immune system also requires:
– Immunoglobulins especially s-IgA, which protects the infant
against infections (14;15)
– Nucleotides which play an important role in growth and
development as they are the building blocks for DNA (14)
– The correct amount of proteins, fats and carbohydrates, vitamins
and minerals for growth and development of the immune system
What happens a few months down the line?
The infant’s immune system continues to develop as the infant
grows with nutrition and environmental factors continuing to play a
role in the further development of the immune system. This process
continues throughout life – even into old age.
Nurture
What can we, as Healthcare Professionals, tell parents to ensure
optimum development of their infant’s immune system?
Nutrition
Healthcare Professionals should emphasise that pregnant women
partake in a healthy balanced diet as it is key to the development of
the foetal immune system. A lack of vitamin A, iron, zinc and
selenium have been shown to impair the immune function and
increase the susceptibility to infection. Pregnant women should
however not take a vitamin A supplement, as it may damage the
unborn child. (See www.eatwell.gov.uk for guidelines on a healthy
balanced diet throughout the life stages).
Prebiotics
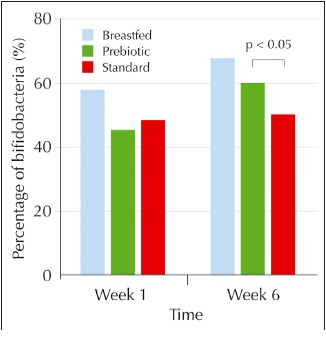
Prebiotics are found in breastmilk and in some infant milk formulas.
A recent study found that the gut flora of babies fed on formula with
prebiotics added was similar to that of breastfed babies. Further
findings from the study demonstrated that babies fed on standard
formula had a lower incidence of bifidobacteria in their stools (12).
(See graph over page).
Breastfeeding is best for babies. Milupa Aptamil First and Milupa Aptamil
Extra are intended to replace breastmilk when mothers cannot or choose
not to breastfeed. It is recommended that infant milks are used only on the
advice of a doctor, midwife, health visitor, public health nurse, dietician
or pharmacist. Milupa Aptamil Forward should be used only as part of a
mixed diet and not as a breastmilk substitute before 6 months.
IMPORTANT NOTICE
*For full copies of the series of advertorials go to
www.milupaaptamil4hcps.co.uk/immunesystem
Breastfeeding is best for babies. Milupa Aptamil First and Milupa Aptamil
Extra are intended to replace breastmilk when mothers cannot or choose
not to breastfeed. It is recommended that infant milks are used only on the
advice of a doctor, midwife, health visitor, public health nurse, dietician or
pharmacist. Milupa Aptamil Forward should be used only as part of a
mixed diet and not as a breastmilk substitute before 6 months.
IMPORTANT NOTICE
Prebiotics help to increase
bifidobacteria to levels similar
to the stools of a breastfed
infant
Prebiotics are found in several
foods such as fruits (bananas
and berries), vegetables
(asparagus, artichokes, greens,
onions, and garlic), legumes
(lentils and kidney beans),
oatmeal and some whole
grains.
Omega-3 fatty acids
Oily fish such as salmon, trout, mackerel, herring, sardines,
pilchards and tuna (not canned) contain omega-3 fatty acids. See
www.eatwell.gov.uk regarding the recommended intake of fatty fish
during pregnancy, breastfeeding and infancy.
Nutritional considerations:
Breastfeeding
Breastmilk is the perfect food, containing just the right amounts of
protein, fats, carbohydrates, vitamins and minerals to support your
infant’s development. It also provides protective substances
including antibodies, prebiotics and nucleotides. In the absence of
breastfeeding, a formula containing prebiotics may help ensure a
baby’s natural immune system is supported.
Weaning
Solids should not be introduced before 6 months (WHO) (however
not delayed after 6 months), but if weaning takes place early then it
should never occur before the age of 17 weeks (16).
– Start with puréed vegetables (root vegetables first), simple
starches and fruit (stewed apples and pears). The
aforementioned foods are beneficial because they are typically
of a low allergenicity and are easily digested
– Introduce a new food every 2-3 days
– If you are from a family with a history of allergies, do not give
foods containing peanut until the age of 3 years (17)
Environment
Environmental factors such as contact with bacteria and infections
may also help to restore the balance between the Th1 and Th2
cells (18).
The panel discussed the negative effects that stress and tiredness
can have on the immune system (19). Changes in maternal hormonal
and immune function as a result of stress in the mother may affect
the infant’s health status, development and function of the infant’s
immune system as physiological stress can suppress both T- and Bcell
functioning, and neurocognitive development of the infant. It is
important for a mother to take time for herself and to get as much
sleep and rest whenever possible for the optimum health of both
mother and child. Stressful experiences or environments very early
in life can alter the responsiveness of the infant’s nervous system
and digestive system and lead to maladaptation of the immune
system throughout life (19).
Conclusion
To conclude, the immune system is continuously developing and
changing throughout life, with a number of critical developmental
changes happening in-utero and during the first few years of life.
These important immunological developmental processes can be
supported by optimum nutrition and appropriate exposure to
environmental factors.
Top line tips for the development of a healthy infant
immune system
• Mother to follow a healthy balanced diet
• Ensure adequate intake of:
– vitamin A, iron, zinc and selenium – pregnant women should
not take a vitamin A supplement
– Prebiotics found in food like oatmeal, some fruit and
vegetables and garlic
– Omega-3 fatty acids in oily fish
• Breastfeed if possible
• If not breastfeeding or if a supplementary feed is needed: A
formula containing prebiotics may be of benefit
• Delay weaning until 6 months if possible (but do not wean
before 17 weeks)
• Families with a history of allergies: Delay the introduction of
peanuts until the child is 3 years old
• Be cough and cold “friendly” as the occasional cough and
cold may help to regulate the balance between the TH1 and
Th 2 cells(18)
• Ensure time for rest and relaxation for the whole family
References
(1) Jones CA, Holloway JA, Warner JO. Fetal immune responsiveness and routes of allergic
sensitization. Pediatr Allergy Immunol 2002; 13 Suppl 15:19-22.
(2) Warner JA, Jones CA, Jones AC, Warner JO. Prenatal origins of allergic disease. J Allergy Clin
Immunol 2000; 105(2 Pt 2):S493-S498.
(3) Warner JA, Warner JO. Early life events in allergic sensitisation. Br Med Bull 2000; 56(4):883-93.
(4) Chien PF, Howie PW. Breastmilk and the risk of opportunistic infection in infancy in industrialized
and non-industrialized settings. Adv Nutr Res 2001; 10: 69-104.
(5) Howie PW, Forysth JS, Ogston SA, Clark A, Florey CD. Protective effect of breast-feeding against
infection. BMJ 1990; 300: 11-6.
(6) Wilson AC, Forsyth JS, Greene SA, Irvine L, Hau C, Howie PW. Relation of infant diet to childhood
health: seven year follow up of cohort of children in Dundee infant feeding study. BMJ 1998; 316: 21-5.
(7) van Odijk J, Kull I, Borres MP, Brandtzaeg P, Edberg U, Hanson LA, Host A, Kuitunen M, Olsen SF,
Skerfving S, Sundell J, Wille S. Breast-feeding and allergic disease: a multidisciplinary review of the
literature (1966-2001) on the mode of early feeding in infancy and its impact on later atopic
manifestations. Allergy 2003; 58: 833-43.
(8) Saarinen UM, Kajosaari M. Breast-feeding as prophylaxis against atopic disease: prospective followup
study until 17 years old. Lancet 1995; 346: 1065-9.
(9) Lochs H. Interaction between nutrition, intestinal flora and the gastrointestinal immune system.
Nestle Nutr Workshop Ser Clin Perform Programme 2005; 10:179-85.
(10) Das UN. Essential fatty acids as possible enhancers of the beneficial actions of probiotics. Nutrition
2002; 18(9):786.
(11) Parvez S, Malik KA, Ah Kang S, Kim HY. Probiotics and their fermented food products are
beneficial for health. J Appl Microbiol 2006; 100(6):1171-85.
(12) Knol J, Scholtens P, Kafka C, Steenbakkers J, Gro S, Helm K, Klarczyk M, Schopfer H, Bockler HM,
Wells J. Colon microflora in infants fed formula with galacto- and fructo-oligosaccharides: more like
breast-fed infants. J Pediatr Gastroenterol Nutr 2005; 40(1):36-42.
(13) Moro G, Arslanoglu S, Stahl B, Jelinek J, Boehm G. Effect of a prebiotic mixture of galactooligosaccharides
(GOS) and long chain fructo-oligosaccharides (FOS) on the cumulative incidence of
atopic dermatitis in infants at risk. Arch Dis Child 2006; 91: A3.
(14) Oddy WH. The impact of breastmilk on infant and child health. Breast-feed Rev 2002; 10(3):5-18.
(15) Brandtzaeg P. Mucosal immunity: integration between mother and the breast-fed infant. Vaccine
2003; 21(24):3382-8.
(16) BDA Paediatric Group Position Statement on Breastfeeding and Weaning on to Solid Foods
December 2004.
(17) Committee on Toxicity of Chemicals in Food CpatE, Department of Health. COT Consumer
products and the environment – Peanut allergy. DoH. 1988. Crown Copyright.
Ref Type: Report
(18) Douwes J, van Strien R, Doekes G, Smit J, Kerkhof M, Gerritsen J, Postma D, de Jongste J, Travier N,
Brunekreef B. Does early indoor microbial exposure reduce the risk of asthma? The Prevention and
Incidence of Asthma and Mite Allergy birth cohort study. J Allergy Clin Immunol 2006; 117(5):1067-73.
(19) Ruiz RJ, Avant KC. Effects of maternal prenatal stress on infant outcomes: a synthesis of the
literature. ANS Adv Nurs Sci 2005; 28(4):345-55.
For further information on the immune system please visit
www.milupaaptamil4hcps.co.uk/immunesystem
or call our careline 08457 623 676
Aptamil Access Code
Thank you for downloading this document from the Aptamil Professional website. Should you wish
to pass this piece onto a colleague, they can gain access to the aptamilprofessional.co.uk website
by entering this code when prompted.
Healthcare Professional Access Code: WSPYRVCHE
