FDA Approves Vemurafenib for Advanced Melanoma
Clinical Context
Melanoma is the leading cause of mortality from dermatologic conditions. In the United States in 2010, there were approximately 68,130 new diagnoses of melanoma and approximately 8700 melanoma-related deaths, according to estimates from the National Cancer Institute.
On August 17, the US Food and Drug Administration (FDA) approved vemurafenib (Zelboraf, Plexxikon/Roche) for first-line treatment of metastatic and unresectable melanomas with V600E mutations in the BRAF gene. This type of BRAF mutation occurs in roughly half of melanomas. The mechanism of action of vemurafenib is to inhibit BRAF, thereby blocking the activity of the V600E-mutated BRAF protein.
Vemurafenib is the second new drug approved this year for treatment of melanoma, the first being the immunotherapeutic agent ipilimumab (Yervoy, Bristol-Myers Squibb), which was approved in March. Along with vemurafenib, the FDA approved a companion diagnostic test, the cobas 4800 BRAF V600 Mutation Test, to detect the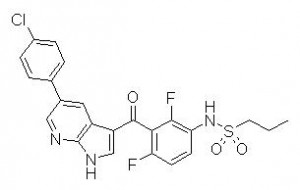 BRAF V600E mutation.
BRAF V600E mutation.
Study Synopsis and Perspective
The FDA approved the oral targeted therapy vemurafenib for the first-line treatment of both metastatic and unresectable melanomas.
The drug is specifically indicated for patients with melanoma whose tumors have V600E mutations in the BRAF gene. An estimated 50% of patients with melanoma have this type of BRAF mutation, which does not occur in normal cells. The drug is not indicated for use in patients without the mutation.
Vemurafenib is a BRAF inhibitor that blocks the function of the V600E-mutated BRAF protein.
Vemurafenib has been approved with a companion diagnostic test that will help determine whether a patient’s melanoma cells have the BRAF V600E mutation. The first-of-a-kind test is known as the cobas 4800 BRAF V600 Mutation Test (Roche Molecular Systems).
“This has been an important year for patients with late-stage melanoma. Zelboraf is the second new cancer drug approved that demonstrates an improvement in overall survival,” said Richard Pazdur, MD, director of the Office of Oncology Drug Products in the FDA’s Center for Drug Evaluation and Research, in a press statement. “In March, we approved Yervoy (ipilimumab), another new treatment for late-stage melanoma that also showed patients live longer after receiving the drug.”
Ipilimumab (Bristol-Myers Squibb) is an immunotherapy also indicated for the treatment of metastatic and unresectable melanoma. Vemurafenib will be marketed differently, as it targets a more specific patient population.
“[The August 17] approval of Zelboraf and the cobas test is a great example of how companion diagnostics can be developed and used to ensure patients are exposed to highly effective, more personalized therapies in a safe manner,” said Alberto Gutierrez, PhD, director of the Office of In Vitro Diagnostic Device Evaluation and Safety in the FDA’s Center for Devices and Radiological Health.
The FDA’s approval of the cobas 4800 BRAF V600 Mutation Test was based on data from the same study that evaluated the safety and effectiveness of vemurafenib.
Vemurafenib was reviewed under the FDA’s priority review program that provides for an expedited 6-month review of drugs that may offer major advances in treatment or that provide a treatment when no adequate therapy exists, says the agency.
Vemurafenib will be marketed in the United States by Genentech and Daiichi Sankyo; rights for the drug were transferred to Daiichi Sankyo when the company acquired Plexxikon, which discovered vemurafenib and codeveloped this new medicine with Roche.
Pivotal Study Details
In a recently presented phase 3 trial, vemurafenib improved progression-free and overall survival, compared with standard chemotherapy, in patients with advanced melanoma with no previous treatment.
Patients receiving vemurafenib had a 74% reduction in the risk for progression (or death), compared with patients receiving dacarbazine chemotherapy (hazard ratio, 0.26; P < .001). Mean progression-free survival was 5.3 months in the vemurafenib group, compared with 1.6 months in the dacarbazine group.
The progression-free survival data constitute “an unprecedented level of difference,” said lead author Paul Chapman, MD, from Memorial Sloan-Kettering Cancer Center in New York City, who presented the data at the American Society of Clinical Oncology (ASCO) annual meeting earlier this year, as reported by Medscape Medical News.
At 6 months, estimated overall survival was 84% (95% confidence interval [CI], 78 to 89) in the vemurafenib group and 64% (95% CI, 56 to 73) in the dacarbazine group. No median overall survival was reported because the data are not mature enough, Dr. Chapman said at ASCO. The study was published in June in the New England Journal of Medicine (2011;364:2507-2516).
In that interim analysis, the median follow-up of the overall survival data was 3.8 months in the vemurafenib group and 2.3 months in the dacarbazine group.
Response rates were 48% for vemurafenib and 5% for dacarbazine (P < .001) in that study, which is known as the BRAF Inhibitor in Melanoma (BRIM)-3 study.
After reviewing the interim analysis, an independent data and safety monitoring board recommended that patients receiving dacarbazine cross over to vemurafenib.
Resistance and Combinations
The complete response rate seen so far with the new drug has been low — just 2 of the 219 patients (0.9%) receiving vemurafenib whose tumor response was evaluated in the pivotal study.
Vemurafenib is also subject to drug resistance, a problem acknowledged by Plexxikon officials.
“Tumor regrowth occurs in many of the patients,” wrote a pair of Plexxikon researchers in a 2010 study about resistance.
A partial solution to this problem might be to combine targeted therapies for melanoma, said a number of experts at the ASCO meeting this year.
A phase 1 trial has already begun with vemurafenib and ipilimumab, reported Dr. Chapman at that meeting.
In addition, a phase 1 study presented there indicated that combining 2 oral targeted therapies, the MEK inhibitor GSK212 and the BRAF inhibitor GSK436, was safe and had preliminary antitumor activity in patients with advanced melanoma.
Adverse Events
In the pivotal BRIM-3 trial, which was conducted at 104 centers in 12 countries, participants had previously untreated, inoperable stage IIIc or IV metastatic melanoma and a V600E mutation in the BRAF gene. Patients were randomly assigned to receive either vemurafenib (960 mg orally twice daily) or dacarbazine (1000 mg/m2 of body-surface area intravenously every 3 weeks).
Common adverse events associated with vemurafenib were arthralgia, rash, fatigue, alopecia, keratoacanthoma, squamous cell carcinoma, photosensitivity, nausea, and diarrhea. Notably, 38% of patients required a dose modification because of toxic effects.
Less than 10% of patients who received vemurafenib experienced problems with high levels of toxicity (grade 3 or worse). The most common of these high-grade adverse effects were skin rashes, photosensitivity, and joint pain.
The investigators also reported that 12% of patients in the vemurafenib group developed grade 3 or worse cutaneous squamous cell carcinoma, compared with less than 1% in the dacarbazine group.
More information on vemurafenib can be found on the FDA Web site.
The BRIM-3 study was sponsored by Hoffman-La Roche. Dr. Chapman reports serving as a consultant/advisor for and receiving research funding from Roche. Other coauthors report financial relationships with industry, including Roche, or are employees of Roche.
Clinical Implications
- The FDA has approved vemurafenib, an oral targeted agent for first-line treatment of both metastatic and unresectable melanomas, and a companion diagnostic test, the cobas 4800 BRAF V600 Mutation Test to identify melanomas with the BRAF V600E mutation. Vemurafenib is indicated only for patients in whom melanoma cells test positive for V600E mutations in the BRAF gene. The dose of vemurafenib given in the pivotal trial was 960 mg orally twice daily.
- Efficacy was shown in a pivotal trial in which 675 patients with untreated late-stage melanoma with the BRAF V600E mutation were randomly assigned to receive either vemurafenib or dacarbazine. Median overall survival time for patients who received dacarbazine was 8 months, whereas median overall survival time for patients who received vemurafenib has not been reached. Estimated overall 6-month survival rate was 64% vs 84%, respectively. Compared with patients receiving dacarbazine, patients receiving vemurafenib had a 74% reduction in the risk for progression or death, and mean progression-free survival time was 1.6 months vs 5.3 months, respectively.
- Common adverse events seen with vemurafenib were arthralgia, rash, fatigue, alopecia, keratoacanthoma, squamous cell carcinoma, photosensitivity, nausea, and diarrhea, but fewer than 10% of patients had grade 3 or worse toxicity. Skin rashes, photosensitivity, and joint pain were the most commonly reported high-grade adverse effects. Grade 3 or worse cutaneous squamous cell carcinoma developed in 12% of patients receiving vemurafenib, but in less than 1% of those receiving dacarbazine. Dose modification was needed in 38% of patients receiving vemurafenib because of toxic effects.
