Giving a Helping Handing in Type 2 Diabetes
Ian Jackson
Former National Health Service (NHS) Prescribing Adviser and Senior Lecturer in Clinical Pharmacology and Therapeutics at a UK Medical/Pharmacy School. Director Green Pill Training Ltd.
Contact: ian.pharmacist@gmail.com
As we have seen from previous articles in this series, guidelines are driven by focusing on targets such as HbA1c which is not without issues as type blood glucose control can increase the risk of hypoglycaemia.
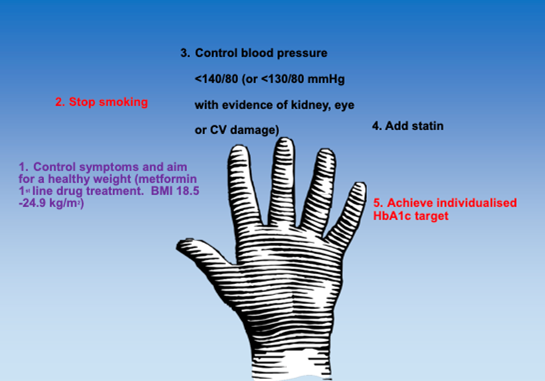
So what should we be focusing on? The Hand of Type 2 Diabetes can give us a helping hand.
First we need to encourage the patient to lose weight if they are overweight or obese. First line drug treatment should be metformin, unless renally impaired, (see future articles). Get the patient to stop smoking if they are smoking. We then need to control their blood pressure, add in a statin (see future articles) and finally target their HbA1c.
Recent studies from the UK are showing the importance of weight loss in overweight type 2 diabetics. The Diabetes Remission Clinical Trial (DiRECT) is a long term study funded by the charity Diabetes UK. (1)
They initially recruited 306 individuals aged 20-65 years who had been diagnosed with type 2 diabetes within the past 6 years, had a body-mass index of 27-45 kg/m2, and were not receiving insulin. The intervention comprised withdrawal of antidiabetic and antihypertensive drugs, total diet replacement (825-853 kcal/day formula diet for 3-5 months), stepped food reintroduction (2-8 weeks), and structured support for long-term weight loss maintenance while the control arm of the study was best-practice care by guidelines.
In the control group there was no weight loss but 24% lost more than 15kg in low-carb group. 4% had remission of type 2 diabetes in control but 46% had remission in low-carb group at 12 months. At 24 months 53 (36%) intervention participants and five (3%) control participants had remission of diabetes. (2)
Discussion.
The findings of the Direct Study has helped altered the care of type 2 diabetics in the UK. All Scottish Health Boards received training to provide the DiRECT intervention for remission of type 2 diabetes in NHS Scotland by December 2019 and in September 2020, a programme was launched to introduce the intervention for 5000 people with type 2 diabetes in selected areas of England. Unfortunately, the Covid pandemic delayed the roll out of this programme.
There are things to consider. In past, we would experience periods of feast and famine. During times of plenty, there are plenty of high carbohydrate foods such as berries and fruits. Consumption of these foods would lead to the release of insulin and these sugars are converted into fats. This stored fat is then broken down during the leaner winter periods or periods of drought. In modern affluent countries people are now consuming carbohydrates constantly throughout the year. The stored fat in no longer broken down and the high levels of insulin release due to high carbohydrate consumption lead to insulin resistance and type 2 diabetes.
The DiRECT study shows how important weight control is and also highlights how we can reverse type 2 diabetes if patients are given support. Give the high levels of type 2 diabetes in MENA areas, it is important to remember to give our patients a helping hand in helping them lose weight before resorting to polypharmacy.
References
(1) Lean M. et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. The Lancet 2018 Feb 10;391(10120):541-551
(2) Lean, M. et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes and Endocrinology. 2019 7(5), pp. 344-355.
